The past year has been a time of great concern and anxiety acutely felt by our behavioral health workforce. Recently we have been overwhelmed by an influx of information about COVID-19 from its risks, testing procedures, and prevention and treatment as well. New and sometimes confusing information about the COVID-19 vaccination is available on the internet and questions and concerns arise from discussions with our behavioral health workforce colleagues.
The most common reasons for reluctance to getting the vaccine are concerns about safety and side effects as well as views that minimize the risk of COVID-19 infection and views of disapproval of vaccines in general.
In the field of medicine, doctors learn that one must weigh the risks of taking a medicine or vaccine against the risk of not taking a medicine or vaccine. In the case of the COVID-19 vaccine, the risk of not taking the vaccine far outweighs the risk of getting the vaccine. COVID-19 vaccines have been held to the same high standards as all other types of vaccines in the United States including the flu vaccine and the vaccine for polio. The COVID-19 vaccines available to us in the USA have been approved by the Food and Drug Administration (FDA) applying the strictest safety and efficacy standards. “The benefit of COVID-19 mRNA vaccines, like all vaccines, is those vaccinated gain protection without any risk of getting sick with COVID-19 from the vaccine” (CDC).
The clinical trials with many thousands of volunteers including elderly have demonstrated that the vaccine is very safe and no deaths have yet been observed or reported from the vaccine (compare that to the estimated 500,000 deaths in the USA from COVID-19). The only serious side effect for some very few individuals has been an allergic reaction which can occur with any new medication or vaccine and can usually be treated medically at the time of the vaccination.
Further, taking the vaccine not only protects that individual – although that alone, the health and well-being of our behavioral health worker is very important, but because COVID-19 is a deadly highly contagious communicable disease, the COVID-19 vaccination will significantly reduce the risk of spreading the deadly COVID-19 virus to family, friends, co-workers and peers as well as the clients we interact with and serve.
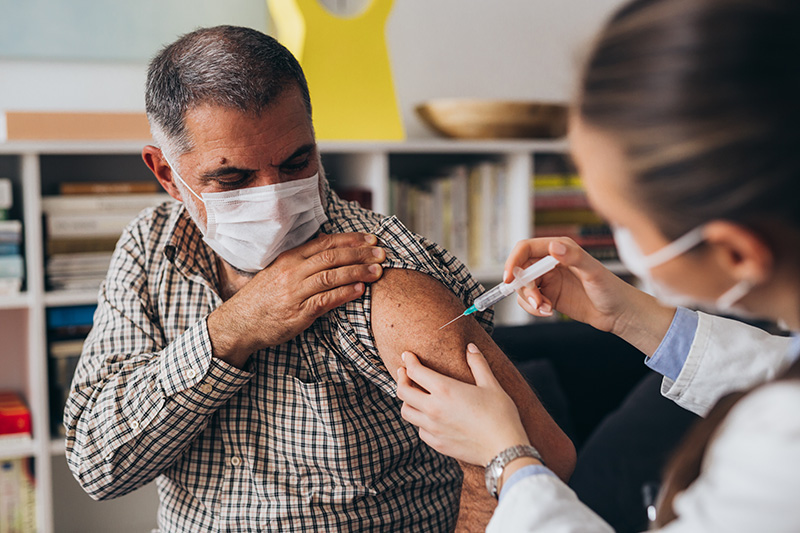
COVID-19 mRNA vaccines are given in the upper arm muscle (deltoid). COVID-19 mRNA vaccines give instructions to our cells to make harmless pieces of what is called the “spike protein.” The harmless spike protein is found on the surface of the virus that causes COVID-19. Next, the cell displays the protein pieces on its surface. Our immune systems recognize that the protein doesn’t belong there and begin building an immune response and making antibodies, like what happens in natural infection against COVID-19. Our antibodies to the spike protein are then rapidly generated upon any exposure to the COVID virus and when they attack the surface protein they kill the virus. At the end of the process, our bodies have learned how to protect against future infection (for 6 months to a year) (CDC Center for Disease Control). Clinical trials have demonstrated that the vaccination protects over 90% of people from getting the infection when exposed, and for those small percentage who do get the COVID-19 infection it is much less severe.
We therefore urge all of our behavioral health workforce colleagues to inquire about opportunities to obtain the COVID-19 mRNA vaccine from their healthcare providers and to discuss any of their concerns or questions.
Gregory Bunt, MD, is Medical Director, Samaritan Daytop Village. He is Past President, New York Society of Addiction Medicine, and is Clinical Assistant Professor of Psychiatry, NYU School of Medicine.




